KevinDailyStory.com – To better understand the risks and benefits of Anterior Cervical Spine Fusion, we examined the patient’s demographics. These factors include age, gender, and body mass index. We also considered a patient’s smoking status, age-adjusted Charleson comorbidity index, and preoperative motor strength. We also analyzed the results of surgical tests. Here are some key details regarding Anterior Cervical Spine Fusion.
Pharyngeal plexus dysfunction leads to narrowing and collapse of the upper airway
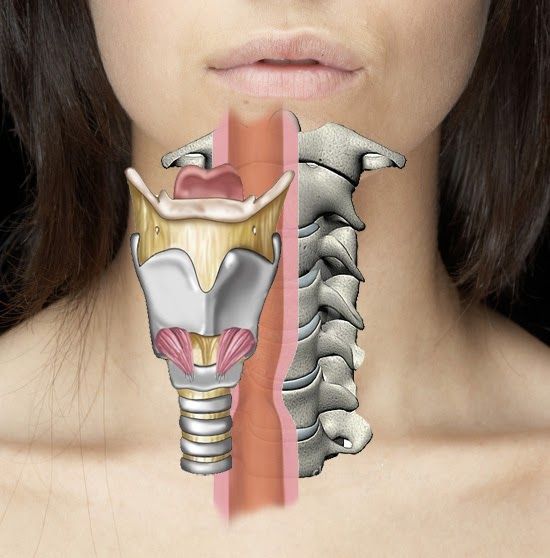
One of the most common spinal procedures in the US is Anterior Cervical Discectomy and Fusion (ACDF). The procedure is associated with a high rate of morbidity and mortality, with the most common immediate complication being dysphagia, attributed to pharyngeal nerve damage. Pharyngeal plexus dysfunction is another risk factor, leading to narrowing and collapse of the upper airway. However, iatrogenic associations with OSA have not been studied.
Anterior Cervical Decompression and Fusion is the standard surgical treatment for radiculopathy and myelopathy. The goal of the procedure is to decompress the nerves and reestablish the physiological height of the intervertebral space and the initial width of neuroforamina. The risks associated with Anterior Cervical Spine Fusion include subsidence of the spacer into the end plate, renewed deterioration, and increased complications.
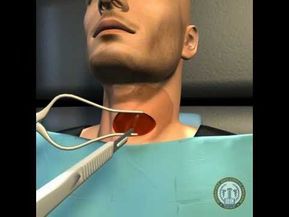
Surgeons can see anterior vertebral bodies
The ACDF procedure requires a transverse incision that extends two to four centimeters. After dividing the cervical fascia in the natural plane, the surgeon can view the anterior vertebral body using a small retractors and an operating microscope. An x-ray is used to confirm that the surgical site is at the correct spinal level. ACDF is one of the most common spinal procedures, and a good patient experience can improve your quality of life.
However, some complications are rare. Patients over the age of 50 years, males, and previous traumatic disorders were at an increased risk of complications. Patients who had more than two levels of surgery were less likely to experience complications. These risks did not reach statistical significance in logistic regression, meaning that the area under the curve was too small to be considered a risk factor. Nonetheless, this procedure has become the standard of care for patients with herniated discs.
Surgery is not a cure for spondylosis
Anterior Cervical Spine Fusion is not a cure for spondylosis, but it can relieve the pain caused by spondylosis. Although the surgical procedure is not a cure for spondylosis, it can help patients recover from their pain and achieve their full potential. The patient should continue to visit his or her doctor to ensure a proper healing. A postoperative physical therapy session should begin about two to three weeks after surgery.
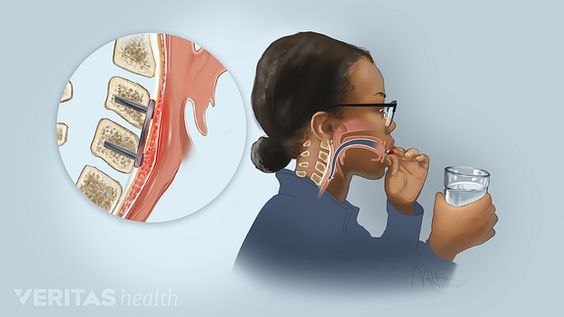
One patient experienced a mechanical failure of an anterior cervical plate screw. He underwent a single level (C7) corpectomy, 360-degree fusion in two settings. A year after discharge, the patient returned complaining of progressively worsening odynophagia, hoarseness, and difficulty swallowing. During imaging workup, the surgeon detected a tracheo-esophageal fistula and inferior anterior cervical plate screw pullout.
0.9% of patients have postoperative wound infection
Postoperative complications of ACDF include postoperative wound infection. One study showed that 0.9% of patients developed postoperative wound infections. Patients’ age and co-morbidity were significant factors. Patients aged 65 to 84 years had an eight-fold increased risk of an adverse outcome. Infections are the most common reason for readmission after ACDF. In addition to the risks, osteopathic patients are at higher risk for OSA.
A three-level Anterior Cervical Discectomy and Fusion with a cervical plate has a poor arthrodesis rate. Despite this, the results of this surgery are largely determined by the type of bone graft used, the size of the plate, and the additional anterior plate fixation. A five-patient study was performed in which patients underwent an anterior cervical discectomy with an autogenous iliac bone graft and an Orion plate to achieve bony union. The patients’ radiological and clinical results were evaluated to assess cervical lordosis and intervertebral disc height.






